What is
Sleep-Disordered Breathing (SDB)?
Sleep-Disordered Breathing comprises a group of disorders characterised by abnormal respiratory patterns or insufficient ventilation during sleep, e.g. apnea and hypopnea. Patients suffering from SDB often may feel exhausted and be unable to concentrate on their daily routine as their sleep patterns are continuously disrupted. Evidence has shown that this may put patients at higher risk for chronic diseases such as hypertension, diabetes, strokes, heart problems and even neurological impairment.
Apnea is defined as the cessation of breathing during sleep lasting ten seconds or more, causing the patient to wake up aroused just enough to take a breath.
Hypopnea is defined as shallow breathing (more than 30% decrease in airflow) for ten seconds or more, together with a lower oxygen saturation or arousal.
Types of SDB
- Obstructive Sleep Apnea
- Central Sleep Apnea
- Complex Sleep Apnea
Obstructive Sleep Apnea (OSA)
This is typically characterised by repetitive upper airway collapse or obstruction during sleep and leading to apneas and hypopneas.
Causes of OSA
- Lack of muscle tone of upper airway structures during sleep, e.g. tongue falling back
- Excess tissue of upper airway, e.g. large tongue, enlarged tonsils
- Structure of the upper airway and jaw, e.g. retrognathic lower jaw
Central Sleep Apnea (CSA)
CSA is much less common and is similar to OSA in that breathing is disrupted during sleep. However, the cause of this is mainly due to the brain not sending proper signals to the muscles that control breathing, unlike in OSA where physical obstruction that coupled with respiratory effort, is the main reason.
CSA may occur as a result of other conditions, such as heart failure, stroke, sleeping in high altitude, etc.
Complex Sleep Apnea
Complex sleep apnea is a combination of OSA and CSA.
Who will likely have OSA?
A recent study by Dr Adeline Tan et al1 found that the prevalence of OSA is higher among Chinese and Malays compared to Indians. The estimated prevalence of moderate to severe OSA for Chinese and Malays was 32.1 per cent and 33.8 per cent, respectively, while it was 16.5 per cent for Indians.
Common Signs and Symptoms of OSA
- Daytime sleepiness / fatigue
- Snoring
- Gasping / choking with sudden awakening
- Headaches upon waking
- Night sweats
- Nocturnal polyuria (excessive urination at night)
- Trouble concentrating
- Forgetfulness / irritability
- Restlessness during sleep
- Sexual dysfunction
Effects of OSA
- Heart problems
- Hypertension
- Stroke
- Arrhythmias
- Cardiomyopathy
- Congestive heart failure
- Heart attacks
- Type 2 diabetes
- Obesity
- Depression
- Sudden death
Left untreated, sleep apnea has also been linked to poor job performance, diminished academic performance, etc.
Diagnosis
Diagnosis of OSA is usually determined with the aid of a polysomnography sleep study, prescribed by a medical specialist, e.g. an Ear, Nose and Throat surgeon or a respiratory medicine physician. Scoring of respiratory events is based upon the 2012 American Academy of Sleep Medicine (AASM) criteria.
Apneas were defined as ≥90% reduction in airflow for at least 10 seconds, and hypopneas were defined as ≥30% reduction in airflow for at least 10 seconds with an oxyhaemoglobin desaturation of ≥3%.
AHI (Apnea-Hypopnea Index) is calculated as the number of apneas and hypopneas per hour of recording time. AHI 5 - 15 represents mild SDB, AHI 15 - 30 moderate SDB, while AHI > 30 severe SDB.
Epworth Sleepiness Scale (Fig 1) is another mode of assessment for OSA. It involves a self-administered questionnaire of eight questions, that when answered properly, aggregates into a score from 0-24. The higher the score, the higher their "daytime sleepiness".
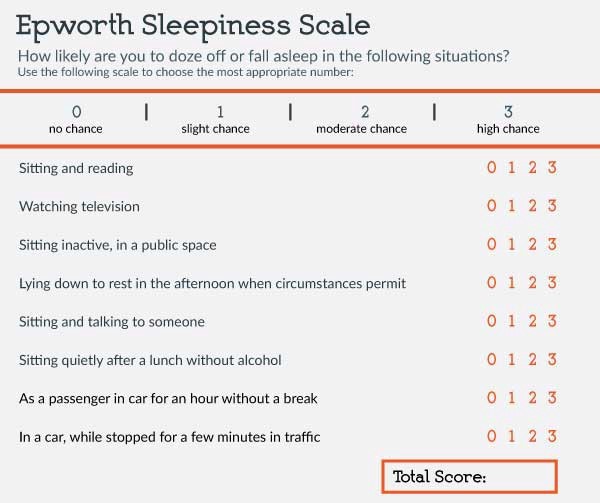
Fig 1 Example of Epworth Sleepiness Scale
Management and Treatment of OSA
- Lose weight, exercise, avoid smoking and alcohol
- Continuous Positive Airway Pressure (CPAP) device
- Oral Appliances
- Mandibular advancement devices (MADs) (Fig 2)
- Tongue retaining devices
- Night guards
- Surgery
- Uvulopalatopharyngoplasty (UPPP)
- Laser-assisted uvuloplasty
- Tonsillectomy and adenoidectomy
- Reduction glossectomy
- Maxillomandibular advancement surgery (orthognathic surgery)
Dental devices have been shown to control sleep apnea long term compared to uvulopalatopharyngoplasty (UPPP), the standard surgical procedure for apnea, in which the surgeon removes soft tissue from the back of the throat. However, dental devices do have some potential drawbacks, including altered bite, teeth movement, pain, dry lips, excessive salivation and in rare instances, arthritis of the temporomandibular joint (TMJ).
Successful management of OSAs is dependent on many factors, including severity of OSA, physical structure of upper airway, medical conditions, personal preference and compliance to regimes.

Fig 2 Example of mandibular advancement device
Services Available at the National University Centre for Oral Health, Singapore (NUCOHS)
When a patient is referred from the sleep specialist, be it a respiratory medicine or Ear, Nose and Throat surgeon, a thorough examination and assessment of the dental structures and oral cavity is performed to determine suitable use of oral appliance. X-rays, assessment of jaw movements, temporomandibular joint health, status of teeth and gums and Mallampati score will be performed for this purpose.
A variety of oral appliances are offered, based on the need and preferences of the patients and these range from hard orthotic oral splint to more complicated mandibular advancement devices (Fig 2) and Herbst appliance.
Review and maintenance visits will be required following the delivery of these appliances, to ensure proper care and usage, to ascertain compliance and successful management of OSA.
References
1. Prevalence of sleep-disordered breathing in a multiethnic Asian population in Singapore: A community-based study. Tan A. Cheung YY, Yin J, Lim WY, Tan LW, Lee CH. Respirology 2016 Jul 21(5):943-50.

Dr Frank Lee
Consultant
Division of Prosthodontics
National University Centre for Oral health, Singapore (NUCOHS)
Dr Frank Lee completed both his undergraduate and postgraduate dental studies in National University of Singapore (NUS) - Faculty of Dentistry in 1997 and 2004 respectively, specialising in prosthodontics. He is also a member of the Royal College of Surgeons (Edinburgh) (Prosthodontics). After three years of advanced specialty training in the National Dental Centre and subsequently, more than ten years of private practice experience, a calling to academia beckoned and he returned to pursue his passion in teaching the future generations of dentists and specialists likewise. He currently coordinates the Crown module in the undergraduate dental program and contributes a fair amount of time supervising their clinics as well. He is involved with the postgraduate prosthodontic programme, sharing his clinical experience and stimulating their inquisitive learning.
Dr Lee is proficient in all areas of prosthodontics, ranging from fixed and removable prosthodontics to complex full mouth rehabilitation, including advanced implant restorative dentistry. He has a keen interest in the field of obstructive sleep apnea, where management using dental appliances are indicated.